May 12, 2022
Watch








Listen
Read
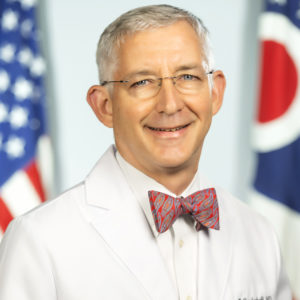
Bruce T. Vanderhoff, M.D., MBA, was appointed director of the Ohio Department of Health (ODH) in August 2021. Dr. Vanderhoff joined the agency after being named chief medical officer in November 2020 and is a key leader in planning, managing, and executing Ohio’s COVID-19 response, including its wide-reaching vaccination program. Dr. Vanderhoff also leads the effort to transform the landscape of public health in Ohio through programs and policies that strive to erase inequities, elevate the importance of social determinants, and improve healthcare access and outcomes.
Before joining ODH, Dr. Vanderhoff had amassed years of experience leading large teams in successfully dealing with important healthcare issues in Ohio. He served more than a decade as a senior vice president and chief medical officer at OhioHealth, where he prepared the healthcare system to manage the threat of Ebola and H1N1. He also addressed pressing healthcare issues affecting Ohio from rural Appalachia to metropolitan Columbus.
His service has made him a nationally recognized physician leader with an impressive track record of managing large-scale healthcare initiatives, addressing disparities, and improving population health.
Dr. Vanderhoff holds a doctorate in medicine from the University of Pennsylvania and a Master of Business Administration from Franklin University. He completed a residency in family medicine at York Hospital in York, Pennsylvania.
Scroll
[00:00:06] Gary Bisbee, Ph.D.: Do you remember Ohio’s successful vaccine lottery? One dose of a COVID-19 vaccine made Ohioans eligible for a random drawing of up to $1 million. To discuss Ohio’s COVID-19 vaccine and masking programs, public health strategy, and lessons from the pandemic, we sat down with Dr. Bruce Vanderhoff, director of the Ohio Department of Health. Dr. Vanderhoff outlined responsibilities of departments of health and the broad role they play in addressing health needs. To solve major public health challenges, like the pandemic, Dr. Vanderhoff begins by understanding the experience of frontline workers and the needs of the public before trying to solve the problems that impact them. We discussed the differences between a primary and secondary booster and whether an annual Coronavirus shot is on the horizon. Dr. Vanderhoff explains the valuable skill of translating science into understandable messaging, a skill he picked up as a family physician. He describes the balance between conveying the seriousness of COVID-19 while also providing hope and direction. For young leaders, dr. Vanderhoff recommends taking advantage of leadership training opportunities, which will encourage introspection and self-improvement.
Well, good afternoon, Bruce. And welcome.
[00:01:35] Bruce Vanderhoff, M.D.: Well, good afternoon. I’m glad to be here with you.
[00:01:37] Gary Bisbee, Ph.D.: We’re pleased to have you at this microphone. This show is about leadership and the pandemic came pretty much right about, I think, when you went to the Department of Health, right? Wasn’t that just about the timing?
[00:01:51] Bruce Vanderhoff, M.D.: Yeah.
[00:01:52] Gary Bisbee, Ph.D.: We were talking earlier, Bruce, and your historical perspective here would be very useful. And we were talking about whatever parallels there might be between this pandemic and the so-called flu. Could you share your thinking about that for us?
[00:02:08] Bruce Vanderhoff, M.D.: Yeah. It’s really remarkable. There are a tremendous number of parallels between this pandemic and that pandemic. For one thing, the pandemic back in 1918 actually lasted a number of years. It had about a three-year run. And by the time that people were reaching about year two, you saw, even then, a lot of fatigue.h You saw a lot of the willingness to take on extra steps or do extra things really begin to fade. You also saw what I think today we would interpret as increasing issues with resilience at all levels of society. And so I think a lot of what we’re encountering or experiencing today m we can look at and say that’s probably just part and parcel of the human experience and how a group of people manage through something as difficult as a pandemic.
[00:03:13] Gary Bisbee, Ph.D.: That’s a really, really valuable perspective, Bruce, that we should not forget, particularly with all the partisan divisions around this. It is an aspect of human experience. Ohio started a very interesting vaccine lottery program that gained a lot of visibility. Can you share with us what led you to that and how did that work?
[00:03:33] Bruce Vanderhoff, M.D.: One of the things that was very clear and very important to us is that there was a big difference between how people who were vaccinated were weathering the storm, compared to people who are unvaccinated. And yet we understood that there were a lot of reasons why people might be hesitant or holding back. And the one thing we didn’t want people to do is not pursue getting vaccinated purely because it was taking some extra effort. So we thought, well, what could we do to create incentives for those who are inclined to get the vaccine, but, you know, they may have other things they want to do that day. How do we reduce that threshold? And the idea of a vaccine grows. And Governor DeWine throughout this has been absolutely committed to being flexible and being creative and doing what can reasonably be done to save as many lives as possible. Very focused on the people of the state. And so as this idea emerged, it seemed like one that might be a good idea. And in fact, it really turned out better than, I think, we hoped it might. If you look at the two weeks and compare the two weeks prior to starting the program to the first two weeks after, we saw a 28% jump in the number of people getting vaccinated. That’s pretty significant. And over the five week window, it was more than half a million people actually lined up to get vaccinated. Keep in mind, this is at a low point in vaccination. We’d just come off the spring and now we were headed into the summer and the virus numbers had gotten really low. And so to get half a million new people showing up to be vaccinated in the five week window really far exceeded our home.
[00:05:29] Gary Bisbee, Ph.D.: Yeah that’s quite amazing. What are the statistics now in terms of number of those vaccinated and number with booster number one, and now booster number two? How is that all working, Bruce?
[00:05:43] Bruce Vanderhoff, M.D.: I think it’s too early to tell regarding booster number two. And as you will recall, the indications for booster number two are different than booster number one. What I can speak to pretty confidently though is what’s going on with the primary vaccine series, the first few shots, and then the followup booster. And what we’re seeing here in Ohio is that, in both instances, we still have operative. But for the primary booster series, we’re now up in the high sixties percentile. So right around that two thirds margin. Would we like to get higher? Yes. And we’re continuing to work to build that foundation of immunity. In terms of then getting a booster, numbers are a little bit lower. But in both instances, we’re continuing to see people, in a sort of ebbing and flowing way, but still a consistent stream of people, thankfully, rolling up their sleeves and getting those vaccines. Now, admittedly, the further we go on, the more of a challenge there is because we’re running into more people who have real reservations about the vaccine or may have just simply decided the vaccine is not for them. But because we know how much of a difference the vaccine has made in outcomes, at least at the Department of Health we have not given up in trying to get the message out about its importance and make the vaccine available.
[00:07:14] Gary Bisbee, Ph.D.: Yeah. What’s the difference, if you could review between the second booster and the primary booster?
[00:07:21] Bruce Vanderhoff, M.D.: So I’ve really come to be the lever to see that first booster as completing the vaccine series. Really, I think, if we look at all the data rolling out, we’re basically talking about a three dose series as your primary vaccination. Now, as we then look at that follow-up data for that fourth dose or the second booster, here’s what it really, in my opinion, is telling us. For a select group of people who are at particularly high risk, there does appear to be some opportunity to add a further boost, or oopmh, that might be the difference between a serious outcome and a less serious outcome. And that’s mostly people that you’d predict, right? People whose immune systems are not functioning at a top level because either of a condition they have or a medication they’re taking. So that group, a group that doesn’t always respond to vaccines as well as the rest of the population. People who are of increasingly advancing age, so the older one one is, and especially if they have a lot of underlying medical conditions. And we see sort of a threshold where that begins to change, those medical conditions begin to really have a significant impact right around 50, and where age itself begins to have an impact right around 65. So I think that fourth dose is an option, particularly for people who, in consultation with their medical professional, are saying, you know what, I’m at higher risk. I’m just going to avail myself into this additional boost.
[00:09:08] Gary Bisbee, Ph.D.: Bruce, will we get to the point, do you think, where there’ll be an annual shot for this Coronavirus like there is for the flu
[00:09:17] Bruce Vanderhoff, M.D.: it’s a little bit hard to make that prediction for one actually very encouraging reason. And that is, it’s very clear from the primary vaccine series that it has resulted in a robust cellular immune response. So a B and T-cell response. The B and T-cell memory can be very long lasting and it may very well be that this primary vaccine series is variable in estimate. Here’s what I’m kind of expecting. I think that the next big driver of a major wave or a major threat to us coming from this virus is going to be yet another novel variant and that being able to add to what we have with primary vaccine series with a novel booster that may be based on some of the more recent variants, including Omicron, in the fall could very well be a booster that is boosting by broadening our immunity and our ability to deal with whatever’s coming next. Will that need to be a regular occurence? I don’t know yet. And I don’t know that anybody knows. But I do, in reading the tea leaves and looking at scientific literature, I’m leaning in the direction of an expectation that there could well be a novel booster for the fall and that it could well prove to be beneficial. But again, a lot of work is going on right now to better understand that and determine if that turns out to be the case.
[00:10:54] Gary Bisbee, Ph.D.: Dr. Fauci, just in the last couple of days, came out with the statement, everybody has to make an assessment of the risk for themselves to make their decisions here. How does that allow you as the director of the Department of Health in Ohio, what kind of flexibility does that give you as you’re talking to the citizens of Ohio?
[00:11:18] Bruce Vanderhoff, M.D.: Yeah. We have been for a long while now taking a very common sense approach to the issue of best guidance for people around dealing with this virus. And as I’ve said now, repeatedly, it begins with the foundation of good immunity, which we believe is best achieved by vaccination. So, hey, if you haven’t gotten vaccinated, please think about rolling up your sleeves and getting that. Beyond that, we’ve also said we are in an era now where everybody needs to apply good, mature common sense to thinking about their medical situation. All of us have to really make good individual decisions about what we’re doing. We now better know, all of us, what the risks are related to this virus. If we’re going to be inside and we’re going to be around people who are spreading the virus, because we know that the viral levels are higher in our community at that time, et cetera, we need to use common sense approaches to protecting ourselves and potentially protecting others. There could be a good reason for me to say at that point, hey, I’m going to put an N-95 mask on because it’s an added layer of protection as I’m trying to deal with this. By the same token, even when the levels are relatively low, as they are now, there are individuals in the community who have immune issues, who have a lot of serious medical conditions, for whom the right answer could very well be wearing a mask now. Look, as Americans, we have always supported each other in terms of being able to make individual decisions and respecting those decisions by individuals. I’m confident that, if you’re in Ohio, as I’m seeing now, people will treat each other kindly and with respect, particularly if people are choosing to continue to wear a mask at this time.
[00:13:17] Gary Bisbee, Ph.D.: Bruce, I know, just from our past dealings, you’re very good at translating science into kind of common speak. But it strikes me that’s probably a really important role for you as a director. Is that true? And how do you think about that?
[00:13:33] Bruce Vanderhoff, M.D.: Well, I thank you for that. That means a lot to me because I do think it’s very important. I think that it’s actually one of the primary roles of the Director of the Department of Health. I have the opportunity, because of the platform that the Governor has provided me with, to message to people what’s happening, hopefully in ways that they can really understand because my experience has been that people make the best healthcare decisions when they personally feel they understand what is happening and they understand what their options are and the best approaches available to them are. And that’s really taken what I did at the bedside as a family doctor for so many years, and simply applied it to this situation and this environment.
[00:14:27] Gary Bisbee, Ph.D.: It seems clear coming out of COVID that the public health actually represents the national economic security of the country. Is that too strong a statement, Bruce? How do you react to that?
[00:14:43] Bruce Vanderhoff, M.D.: Well, I’d react by saying there’s no questions are intertwined. The health of the community, the health of the people of the state or of the nation, has a direct impact on our readiness and ability to respond to just about anything, whether it’s our ability to respond to COVID, and the data has been very clear on that. The healthier you are, the better you’re able to weather the COVID storm. So what can we do to help as many people be as healthy as they can be so they can better weather the storm? That’s true as we broaden that and think about, well, what about our economic vitality? Well, the more of us who are well and able able to engage in our workplace and engage in our communities, hey, the better off all of us are.
[00:15:36] Gary Bisbee, Ph.D.: So you have your medical degree, obviously. You’ve also got an MBA. But I suspect, in this position, you have to think like a lawyer. Is that true? I mean, how do you kind of react to all the rules and regulations of the state and the nation here?
[00:15:54] Bruce Vanderhoff, M.D.: Yeah. I think it’s a very important component of leadership, whether it’s leadership at the state level or it’s leadership at a hospital or in your local community, or even in your own practice because those rules are really the grease that allows our communal life to function. And while sometimes they’re frustrating and sometimes they can even be daunting, we do, to your point, really have to try to understand them and be mindful as we’re making decisions and trying to chart a course for the future, about the guardrails that those are providing us with. And to the extent that we may find the guard rails don’t make sense anymore, our understanding of them then gives us the opportunity to work to improve or modify this guardrail. So I think that’s a very good insight, Gary, and agree with it completely.
[00:16:53] Gary Bisbee, Ph.D.: Okay. How do you balance positiveness and hope? You’re a very positive person anyway, but how do you balance positive and hope with the seriousness of the pandemic for your citizens in the state?
[00:17:08] Bruce Vanderhoff, M.D.: I think that it’s a big mistake to not understand the risks, the dangers. And to communicate honestly about those, you have to acknowledge that. You also have to acknowledge the pain and the loss that people are experiencing. Those are very real. They are part of our shared experience. They’re part of individuals’ lived experience. But it does not help the patient. It does not help the community to linger there or to separate on that. But what people need from their leaders is then, okay, understanding that, what’s the hopeful course into the future? How do we navigate this towards success, because I think that’s where you can really make a difference. Understanding for real what people are going through, but then say it’s all right. It’s not what any of us wanted, but it’s where we are now. Let’s take the information we have and let’s navigate our way out of this the best we can.
[00:18:21] Gary Bisbee, Ph.D.: Bruce, how did the department work with hospitals and health systems in the state?
[00:18:27] Bruce Vanderhoff, M.D.: Well, it was very, very clear as we were entering this pandemic that partnership and working closely with the hospitals was going to be absolutely essential to our success. And prior to my arrival, Governor DeWine had really taken a step that I think is fairly unique in the country in establishing the zone system. Now it was a zone system, three zones. They were built on the regional emergency response systems that I know many states have. But we took it a step further by creating three defined zones, each with a physician leader who was tasked with working closely with all those hospitals and health systems in their zone, and in turn, those folks had representation for all of the regions. So it really allowed us, on an almost daily basis to have collaborative interactions with healthcare leaders, especially hospital leaders, around the issues that we were all working through, contending with, etc. And without going into a lot of detail, what I can say at a high level is that kind of collaborative engagement was game changing because it enabled us to be very surefooted and yet responsive as we were dealing with a host of unanticipated events and issues.
[00:19:53] Gary Bisbee, Ph.D.: What lessons will public health officials take from the whole pandemic?
[00:19:58] Bruce Vanderhoff, M.D.: Well, I’m sure that we will take many. And without trying to catalog all of them, there are a few that really stood out for me. One is, I think, a recognition that we cannot possibly predict, with accuracy, all the threats that we could face in dealing with public health. But there is something that we do know today that we have to continue to lean hard into, and that is people who are healthy can weather a pandemic or other health challenge better than people who are not healthy. And so I know, here in Ohio, we’re very focused on, what are the further steps that we can take to improve the overall health of the people of Ohio and recognize that that is a crucial part of our preparation for whatever comes next. And I think, heretofore, people in public health had often viewed those as two separate but important issues. I think now there’s a growing recognition that they are intertwined issues, part of each other. The other lesson that I think we’ve taken from this is the incredible importance in this day and age of highly developed data and analytics systems, systems that can talk to each other, and reducing as much as possible our reliance on sort of hand counts and paper records and paper reporting or non electronic reporting, automating things as much as possible. Not only is it more accurate, but it really allows for a level of analysis that is really important. So I think you see nationwide major investments beginning at the federal level in a data modernization effort.
[00:21:53] Gary Bisbee, Ph.D.: You and other public health officials have been at the forefront of leadership decisions during this pandemic. And all of you are due our respect for sure. What was life like growing up for you, Bruce?
[00:22:09] Bruce Vanderhoff, M.D.: Well, I consider myself very fortunate. I was raised in a large loving family that had a deep and abiding faith. And one of the things that I can remember my parents saying to me over and over and over again was, to whom much is given, much will be required. And it always struck me because we weren’t wealthy. So, I mean, I knew as a child, they were talking about other guests. They were talking about the other things that I had been blessed with, which was a good mind, a good family, caring people around me, a good education, et cetera. And so I’ve always been very mindful of that and that influence growing up really has had a very big impact on my decisions of whether they were what kind of medicine to specialize in or how to make decisions about my career.
[00:23:17] Gary Bisbee, Ph.D.: Well, what did the young Bruce think about leadership?
[00:23:21] Bruce Vanderhoff, M.D.: That’s interesting. When I was a boy, I was very, very shy. And I was far more likely to sort of think about things than to act on them and to engage in. I fortunately had a wonderful teacher in sixth grade. Her name was Mindy Weinberg and she really invested in me. And she said to me more than once something along the lines of, Bruce, if you wait for people to see what you are bringing to the table or if you don’t step up and essentially provide leadership, people are going to go right past you. And that’d be a shame because you have a lot to contribute and I’m not going to let that happen while you’re under my watch.
[00:24:19] Gary Bisbee, Ph.D.: Good her.
[00:24:20] Bruce Vanderhoff, M.D.: She pulled me out of my shell. She pulled me out of my safe place of being a shy introvert, and set me on a path of then linking this to what I was raised with, the notion that to whom much is given much will be required. And I said, inside myself, I got to make, I got to change. And immensely grateful to her. And many times in my life, went back to her grade school classroom just to visit and thank her for the difference that she made in my life.
[00:24:58] Gary Bisbee, Ph.D.: Oh, that’s very cool. I’m sure she really appreciated it. But that’s pretty heady stuff for a sixth grader, Bruce.
[00:25:05] Bruce Vanderhoff, M.D.: It is and, believe me, it had a huge impact on me. At first it was almost like an intervention, this teacher saying this to me. But I knew it was coming from a place of real caring and that this was coming from somebody who wanted all of her students to be the best they could be. I knew that. And so I was willing to look inside and say, okay, what does this mean? What do I have to do differently than what I would otherwise do?
[00:25:39] Gary Bisbee, Ph.D.: So you mentioned your parents and the loving nature of the family, but do you think your parents contributed to your leadership style?
[00:25:47] Bruce Vanderhoff, M.D.: I do because I think I learned from them that a leader does not have to be someone who is bombastic, does not have to be somebody who is aggressive, but can really be somebody who sets a course or helps lead people in a direction by caring about them. Helps them see a future direction because they’re willing to go on that path themselves and they are encouraging other people to come with them because that’s the way that my parents treated me.
[00:26:26] Gary Bisbee, Ph.D.: So moving on, you mentioned medicine, of course. You went to Penn biology degree, basically. At what point did you decide on medicine as a career, Bruce?
[00:26:37] Bruce Vanderhoff, M.D.: Well, it’s interesting. So when I went to college, I had no idea of what I wanted to be. And I explored very seriously a number of degree paths, including real interest in anthropology, a real interest in history. But I really fell in love with the neurosciences and the degree at Penn that is now called neuroscience. It was actually, at that time, called biological basis of behavior. But it was a neuroscience degree. And so I just really loved the neurosciences. And I envisioned a career in the neurosciences and medicine. That’s what drew me in. That path changed during the course of medical school because I also, in the course medical school, really fell in love with the clinical side of what a doctor does. I fell in love with the doctor patient relationship and a doctor’s ability to really impact the lives of the patients that he or she serves. Through that relationship, and in my case did something that at Penn was fairly unusual at the time and said, I think I’m going to be a family physician based on some experiences, some special rotations I was able to take as electives in family medicine out in the community. But again, it was all driven by a lot of these things you and I have talked about.
[00:28:12] Gary Bisbee, Ph.D.: Well, interesting. You were in practice as a family practitioner, of course, and then made a decision to go to OhioHealth, which resulted in your being the Chief Medical Officer there. What was the sequence of steps, Bruce, that you went through to go from family practice to become the CMO at OhioHealth?
[00:28:31] Bruce Vanderhoff, M.D.: Well even when I had finished with my residency and was heading out into private practice in Ohio, which was a good choice because it’s where my wife was from. And so it gave us an opportunity. She’d been with me for a long time in Philadelphia. And so it gave me an opportunity to get back onto her turf. But even as I was doing that, my residency director said to me, Bruce you really like to be involved in teaching and sort of the science of medicine and I think you’re going to end up in medical education. And I thought, well, of course you’re saying that because that’s what you’re in, but you are wrong. Well, no, he was right. Dr. Dick Sloan, he’s still alive today. And he was right. And so that’s how I ended up at Ohio State, and from Ohio State, at OhioHealth, because OhioHealth had an opportunity. They were looking for an associate residency director and I took that role. And from there, became very interested in quality and quality improvement. And again, it all hearkened back to these things I was talking about, what could I do that would have the most impact for the most patients? And I really saw improving the quality of the care we deliver and doing it in partnership with the other members of the medical staff, helping this be a shared journey as opposed to something that was imposed. So I got deeply involved in that, had no plan whatsoever for an administrative career. But in the midst of doing that, became more and more involved in medical administration at my hospital through the lens of the quality work that I was doing and discovered that I had a facility at working with both the administration and the medical staff to help get things done and get it done as a team, as opposed to necessarily trying to get it done as one group versus another, working through different courses, but trying to stay together on a common course. And then eventually that led to rising to be the Chief Medical Officer of a large midwest health system. And I was privileged to do that for almost 13 years.
[00:30:50] Gary Bisbee, Ph.D.: Well from one substantial leadership position at OhioHealth to another, at the Department of Health. And what was the thinking, Bruce, that kind of took you from OhioHealth to Ohio state?
[00:31:04] Bruce Vanderhoff, M.D.: Well, I think it all circled back to what we began with. I was incredibly blessed by the role that I served in for so many years at OhioHealth and I had really a medical family there that supported and embraced me. And I remain, to this day, immensely grateful for all the people there and all the opportunities I was given. But I. for a number of years, was feeling this calling. To whom much has been given, and I had been given much, much will be required. And I really felt that the lord was calling me to do more.
[00:31:45] Gary Bisbee, Ph.D.: What is your role as the director? What are the kind of the basic functions of the director? I suspect a lot of us aren’t actually that familiar with that role.
[00:31:55] Bruce Vanderhoff, M.D.: Yeah. So when I was tapped to do this and make this change, I didn’t really know either. I felt that I saw what was happening and I knew that there was a real opportunity in public health and public health at the state level to make a difference. And so in the course of it, I I stepped into it not fully knowing, but what I’ve come to know now is that the Department of Health not surprisingly plays a broad role. in addressing the health needs of the people of the state and advancing health initiatives. Just to give you an idea of the scope of the Department of Health, our budget is well in excess of a billion dollars, and we are involved in everything from the survey and accreditation of institutions that deliver healthcare across the state to the development of programs at a frontline level that address things like reducing lead toxicity in children, addressing infant mortality, improving issues that relate to aging, and I could go on and on. So, a really broad range of things. But the good news for me is they’re all directed toward improving the health of the people of the state.
[00:33:19] Gary Bisbee, Ph.D.: Thinking back to your time at OhioHealth in various capacities there, but clearly as the Chief Medical Officer, what learnings did you take from that role, Bruce, that you were able to apply to the director role here?
[00:33:35] Bruce Vanderhoff, M.D.: Two that really stand out for me. The first is, if you really want to get big things done, you have to both be willing to work with people towards that goal and you have to design a path that is stepwise, that’s iterative. You can’t solve big problems in one giant step. You have to break it down into a journey that brings people with you. The second thing that I learned is just how important it is to understand the lived experience of people who are involved with what you’re trying to address. You can’t start out thinking you know the answers. You have to take a moment and dive in to understanding what the people on the front lines know and are experiencing before you formulate what you think are going to be the plans. And then you work with them to identify the plans for how to solve it.
[00:34:45] Gary Bisbee, Ph.D.: Now that you’ve been Director of Health for the state of Ohio, looking back to your time or thinking back to your time when you were the CMO of a large health system, what do you wish you had known then?
[00:35:01] Bruce Vanderhoff, M.D.: Looking back, I think the thing that I learnt the most along the way, and I wish I had known at the beginning, was how vital, how important it is to establish the kind of systems of interaction and organization that create the well-oiled machine. And it’s not to say that I didn’t work on those things earlier in my career. It’s not to say that I didn’t have the benefit of some good committees and workspaces and organizations. I did. But what I have seen as I’ve moved through not only my career, but this pandemic, is how vital it is to have a highly evolved organization and how vital it is for everyone in the healthcare delivery system to be talking and working together to address challenges.
[00:36:09] Gary Bisbee, Ph.D.: Great advice. Bruce this has been an absolutely terrific interview. Just really first-class. So thank you for your time. I have two other questions if I could. One of them is for those young people thinking about going into public health as a career, and usually these kind of high visibility crises like this pandemic does draw people in, but what advice would you have for a young person thinking about a career in public health?
[00:36:39] Bruce Vanderhoff, M.D.: Well, really two things that I think you should really think about very carefully. One is, don’t neglect the clinical opportunities you have early in your career to really engage in direct patient care experiences because, in large part, they’ll help inform your leadership later. They’ll help you to really understand how the people you’re working with are experiencing their professional work, their health work. So that’s one. The other is that, as you’re thinking about a career in public health, recognize how important communication is and invest in and take opportunity to hone your communication skills, to gain opportunities, to provide interviews, to be on camera, to perhaps be on the radio. Those are invaluable because they’ll help you to be the most effective public health leader that you can be.
[00:37:48] Gary Bisbee, Ph.D.: For up and coming young leaders, not necessarily in public health, but in any aspect of healthcare, for up and coming young leaders, what advice would you have for them, Bruce?
[00:38:00] Bruce Vanderhoff, M.D.: TAke advantage of leadership training opportunities, even though as you are working through your day to day, you may see those as, oh, just one more thing you have to do. The reason I think they’re so important has I think less to do necessarily with perhaps all the course content that they might cover, but more to do with the introspection that they will afford you. They give you an opportunity to, in a structured way, think about and engage in self-improvement that will put you in the best position for success as a leader as you go forward. They’ll also pass on to you some of the important tips that everyone needs to have if you want to avoid repeating the mistakes of the people who went before you.
[00:38:54] Gary Bisbee, Ph.D.: Bruce, great advice. We really appreciate your time today, and I appreciate your friendship through the years. Thank you.
[00:39:02] Bruce Vanderhoff, M.D.: No, thank you. It was great to be with you and I really enjoyed it.